There are 3100 patients currently recruited to the TRIGS trial. There will be six countries and more than 40 sites participating in the TRIGS Trial. The TRIGS -D trial and a cancer recurrence sub-study will be a sub-study of the main trial.
Study intervention
A bolus of study drug, 0.15 ml/kg (TxA 15 mg/kg or matched placebo) before surgical incision, and then infusion at 0.05 ml/kg/h until the end of surgery. All other aspects of anaesthesia and surgery are flexible.
Primary endpoint
Surgical site infection.
Secondary endpoints
Include red cell transfusion, other healthcare-associated infections (pneumonia, blood stream infection, etc.), and the number of days at home within 30 days of surgery (DAH30).
Safety endpoints
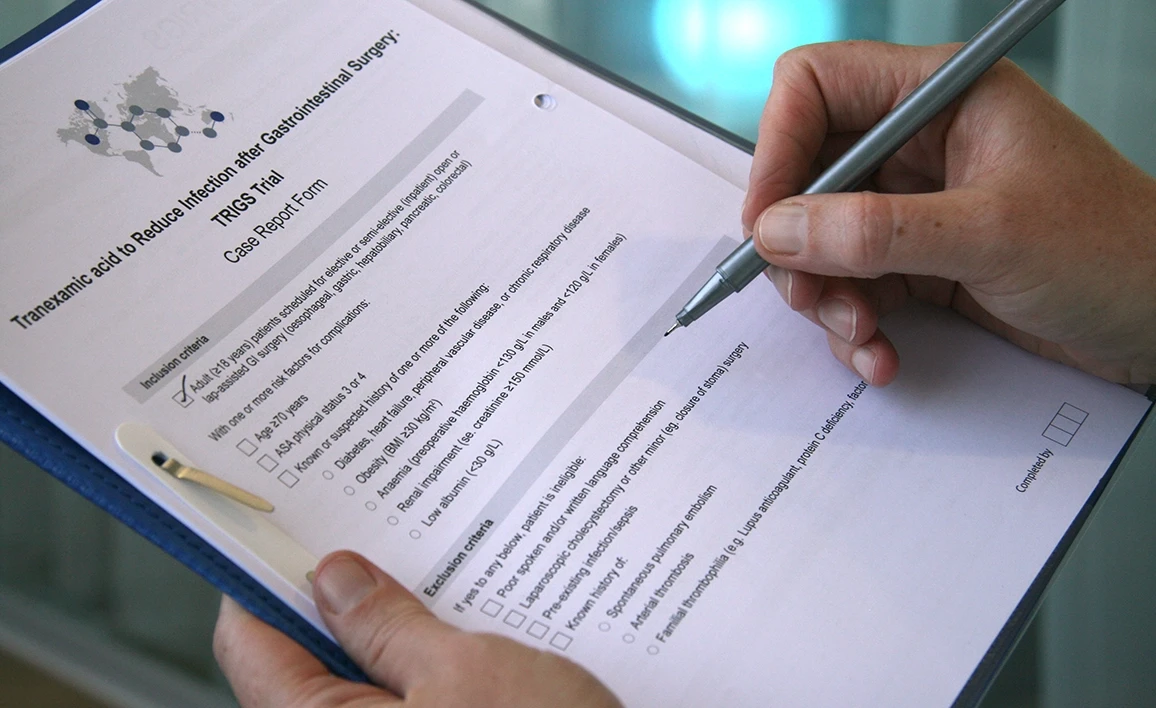
Myocardial infarction, stroke and thromboembolic events; other adverse events. Entry criteria: adult patients scheduled for elective or semi-elective open or lap-assisted gastrointestinal surgery (oesophageal, gastric, hepatobiliary, pancreatic, colorectal) with one or more risk factors for complications.
Sample size
3300 patients.
Study duration
Five years.
The Australian National Health and Medical Research Council (2020): $A5197000
ANZCA Foundation (2021): TRIGS-D sub study $A120000
The CLIP-II study is endorsed by the Australian and New Zealand Intensive Care Society Clinical Trials Group (ANZICS-CTG), the ANZCA Clinical Trials Network, and the Australian and New Zealand Society of Cardiac and Thoracic Surgeons.
ClinicalTrials.gov Identifier: NCT04192435
$A1000
Principal Investigator
Paul Myles
Co-Investigators
Robert Sanders, Lisbeth Evered, Mark Shulman, Wendy Brown, Stefan Dieleman, Tim McCulloch, Robert Medcalf and Jessica Kasza
Trial summary
Delirium is a devastating complication of medical and perioperative care, associated with increased morbidity and mortality, dementia and impaired long-term cognition, and loss of independence. Delirium is also associated with neuronal injury placing patients at risk for long-term changes in cognition. There are no proven therapies for postoperative delirium, mainly due to the lack of adequately powered, biologically plausible trials. There is growing evidence that tranexamic acid (TxA) may reduce inflammatory pathways in the central nervous system and protect the blood-brain barrier in trauma, and surgery.
TRIGS-D study aims
In a subset of 826 patients randomised in the TRIGS trial, we will collect data on delirium incidence and severity. Our specific aims are to investigate whether TxA:
- Aim 1: Reduces the incidence of postoperative delirium diagnosed with the 3D-CAM.
- Aim 2: Reduces the severity of delirium diagnosed with the 3D-CAM-Severity (3D-CAM-S).
- Aim 3: Modulates inflammatory (plasma cytokines, innate cell immune profile) and neurophysiological (EEG) responses in concert with any alteration in the incidence or severity of delirium.
- Aim 4: Reduces longer-term impairment of quality of life and improves disability-free survival.
Primary hypothesis
Prophylactic TxA administration in patients undergoing major gastrointestinal surgery reduces the incidence of delirium after surgery when compared with placebo. The unifying hypothesis is that systemic and neuro-inflammation lead to neuronal injury and resultant postoperative delirium.
Study Design
Multicentre, randomised, triple-blind, placebo-controlled, clinical trial (a substudy of the TRIGS trial). Patients are randomly assigned to either TxA or matched placebo. The incidence of postoperative delirium will be assessed daily using the 3D-CAM or CAM-ICU and medical record review for the first 3 days after surgery. In addition, follow up assessments will be done at 30 days and 12 months.
Funding source
The Australian National Health and Medical Research Council project grant (ID 1185145) and the Australian and New Zealand College of Anaesthetists (22/002).
| Australian hospitals |
| Alfred Hospital |
| Austin Health |
| Blacktown Hospital |
| Cabrini Hospital |
| Epworth Hospital |
| Peninsula Hospital |
| Gold Coast Hospital and Health Service |
| Gosford Hospital |
| Goulburn Valley Health |
| Grampians Health Ballarat (previously Ballarat Health Services) |
| Logan Hospital |
| Mackay Base Hospital |
| Monash Medical Centre |
| Northern Health |
| Peter MacCallum Cancer Centre |
| Prince of Wales Hospital (NSW) |
| Princess Alexandra Hospital |
| Redcliffe Hospital |
| Rockhampton Hospital |
| Royal Adelaide Hospital |
| Royal Brisbane and Women's Hospital |
| Royal Hobart Hospital |
| Royal Melbourne Hospital |
| Royal Prince Alfred Hospital |
| Sir Charles Gairdner Hospital |
| St John of God Hospital (Subiaco) |
| St Vincents Hospital, Melbourne |
| The Avenue |
| The Tweed Hospital |
| University Hospital Geelong - Barwon Health |
| Werribee Mercy Hospital |
| Western Health Service |
| New Zealand hospitals |
| Auckland City Hospital |
| Waikato Hospital |
| Te Whatu Ora Waitemata- North Shore Hospital |
| International hospitals |
| Vanderbilt University Medical Center |
| Tuen Mun Hospital |
For further information about this study, please contact the TRIGS Project Manager, Sophie Wallace by email.